By Lynn McCain
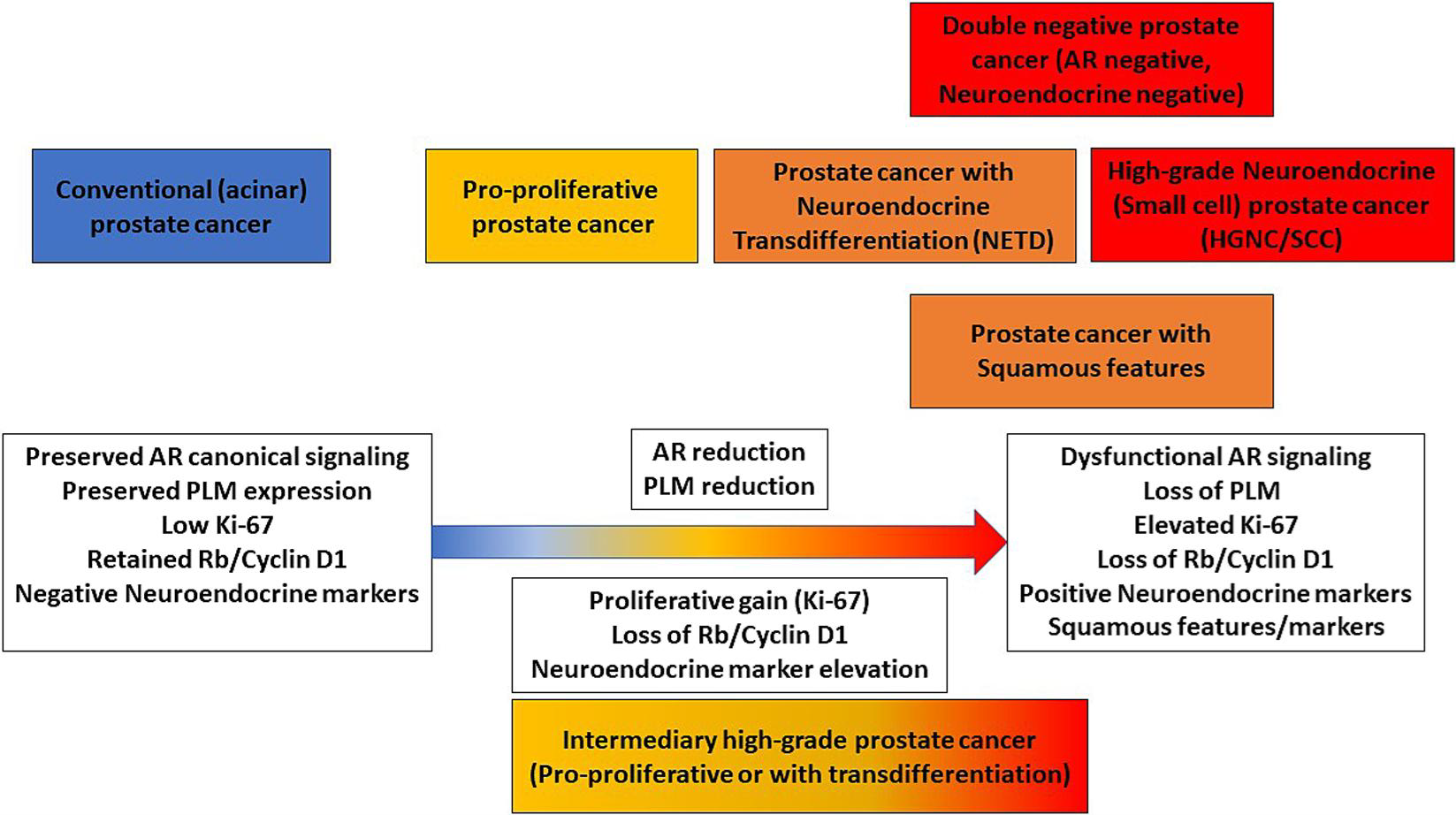
The diagnosis of metastatic prostatic cancer (MPC) by fine needle aspiration (FNA) can usually be rendered by examining the cells’ shape and appearance under a microscope (its cytomorphology) and through features seen in immunohistochemical (IHC) testing. However, when patients have undergone androgen deprivation therapy (ADT) or cells have undergone other types of pressures, MPC diagnosis may be complicated as the cells may transform into other abnormal types such as small cell carcinoma. To aid in the diagnosis of MPC, predictive and prognostic biomarkers can also be assessed by IHC.
A research team from the Michigan Center for Translational Pathology undertook a study to illustrate how careful assessment of cytologic and biomarker features may provide physicians with information on MPC patients’ prognosis and the best therapies to consider.
They found that aggressive cytomorphologic variants were commonly identified in patients with prior ADT. Identification of nonconventional cytomorphology and increased proliferation can provide important information regarding the patient’s prognosis. Recognition of these changes is important for an accurate diagnosis, and the identification of high-grade variants can affect therapeutic decision-making. In addition, they found that clinically actionable biomarkers such as PDL1 and ARv7 can be assessed by IHC, which can help guide therapeutic decision-making by physicians. These findings were recently published in Cancer Cytopathology.
Full citation:
Cantley, RL, Wang, X, Reichert, ZR, et al. Metastatic prostate cancer diagnosed by fine needle aspiration: contemporary cytopathologic and biomarker assessment with clinical correlates. Cancer Cytopathol. 2022; 1- 19. https://doi.org/10.1002/cncy.22652