MEDICARE (CMS) LAW
Under Medicare (CMS) law, MLabs cannot bill Medicare for technical charges if the order date is less than 14 days after the patient was classified as a hospital inpatient or outpatient, or was an inpatient in a Skilled Nursing Facility (SNF) in a Medicare paid bed, except for molecular pathology testing (CPT code range 81105 - 81479) collected from a hospital outpatient. See the chart below.
If a specimen was obtained in a private physician office (not billing under a facility tax ID), MLabs can bill Medicare directly for both technical and professional services (unless the patient was also in a SNF Medicare paid bed on the date of service or hospice).
MEDICARE 14-DAY RULE
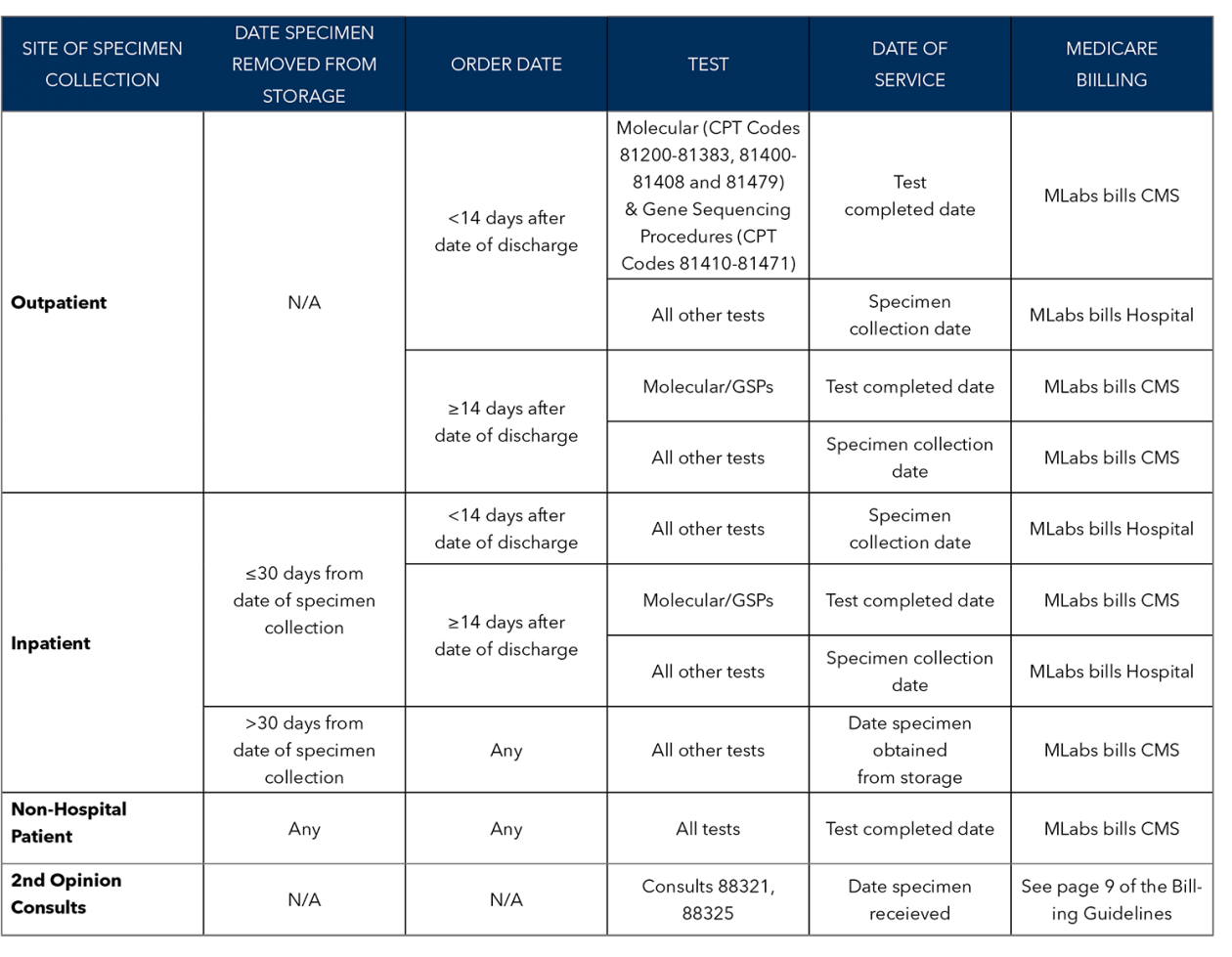
BILLING SCENARIOS
TRADITIONAL MEDICARE EXAMPLES
|
|